- Pulse Biosciences (PLSE) started in 2004 with its Nano-Pulse Stimulation (NPS) technology, and hasn’t found any success in over 20 years. It failed its dermatology application in 2021, then abandoned it and went into the Pulsed Field Ablation (PFA) cardiac market in 2022.
- Today, 3-years later, the company has made little progress in developing its technology for the PFA market and is making another transition to Benign Thyroid Ablation. This market is small, and looks to be another dead end for PLSE.
- PLSE’s own paid consultant and investigator of trials, Dr. Vivek Reddy, who owns stock/options in PLSE, has stated that there’s likely no benefit with nano-pulse PFA over micro-pulse PFA. And if there is any benefit, it would be a niche one but that “still remains to be proven”.
- Early PLSE clinical data on thyroids are of poor quality and the outcomes suggest inferior performance vs the competition.
- PLSE has lost three CEOs over the past three years, and the company doesn’t say why. We logically speculate the reasons.
Pulse Biosciences History Of Failure Will Likely Continue
Pulse Biosciences (PLSE) is a speculative MedTech company that has not made any material revenue over the past 20 years with their Nano-Pulse Stimulation (NPS) technology. They started in the oncology field, then pivoted to dermatology. As stated from a Google search:
In 2004, Pulse Biosciences was focused on developing and commercializing medical devices for ablative treatments, particularly in the oncology field. The company was developing its proprietary Nano-Pulse Stimulation (NPS) technology, which would later become the foundation for its CellFX System. The CellFX System is used for dermatologic conditions, leveraging the non-thermal nature of NPS to address areas where traditional solutions are limited.
Source: Google
18 years later, in 2022, PLSE realized that their NPS technology wasn’t marketable to treat dermatology conditions. It then pivoted to a new field that was booming – Pulsed Field Ablation (PFA) in cardiac applications. Since PLSE’s PFA development was moving slow relative to competitors, PLSE again pivoted to use its NPS to treat benign thyroid ablation.
Pulse Biosciences Competitor Kardium Recently Announced Stellar Results for Its PFA Catheter
Kardium is a private company that, like PLSE, is developing a catheter system for PFA. However, unlike PLSE, Kardium has some real innovation. Its Globe PF System is their catheter, much more advanced than PLSE’s basic catheter.
On 4/25/25, Kardium announced in a PR:
These pivotal findings from the PULSAR IDE study were announced at the Heart Rhythm Society (HRS) meeting in San Diego1, highlighting the safety and efficacy data of the Globe PF System, which is currently under PMA review with the US FDA.
“These impressive one‑year efficacy results underscore the advanced catheter design of the Globe PF System,” said Dr. Vivek Reddy, Co-Principal Investigator from The Mount Sinai Fuster Heart Hospital, New York. “Given the excellent durability achieved by the Globe PF System, the efficacy result is likely approaching the limit of what we can achieve with PV isolation alone.”
Dr. Vivek Reddy is one of the nation’s premier cardiac electrophysiologists. He is a consultant for many companies in the PFA field, including PLSE and Kardium. His statement above about Kardium is a lot stronger than what he said regarding PLSE.
The following is what Dr. Reddy reported about PLSE in January 2025 regarding being an investigator for their feasibility study:
“The remap results for the first 30 patients treated with the Nanosecond PFA 360° Cardiac Catheter demonstrate strong pulmonary vein isolation (PVI) with short case times,” said Vivek Reddy, MD, Director of Cardiac Arrhythmia Services at the Mount Sinai Fuster Heart Hospital, NY. “This novel technology offers a unique user experience that has the potential to improve workflow with a pliable catheter for nimble and precise positioning in the anatomy, and combined with the differentiated energy, enables consistent, durable transmural ablations.”
Look at the difference between the two statements by Dr. Reddy. For Kardium, he talks about the “advanced catheter design” and “excellent durability achieved by the Globe PF System”. He praises Kardium’s specific system.
For PLSE, he says “potential to improve workflow with a pliable catheter”, not mentioning that PLSE’s Nanosecond PFA 360° Cardiac Catheter is anything special. His tone is neutral at best in regards to the PLSE 360° Catheter’s limitations.
Dr. Vivek Reddy, Pulse’s Own Hired Consultant, States There Isn’t An Advantage To Using Nano-second PFA Compared to Micro-Second PFA For Most Procedures
Dr. Vivek Reddy did a presentation at the 29th Annual International Atrial Fibrillation Symposium, showcasing his work on PLSE’s feasibility study. This was in February 2024. At the :21 time mark, Dr. Reddy discloses that he has an equity stake/stock options in PLSE, Kardium, and a slew of other MedTech companies in the PFA field.
Starting at the :30 time mark, Dr. Reddy describes PLSE’s catheter. Presentation slide below:

Source: AF Symposium 2024 presentation
PLSE’s catheter is far from being approved for commercial use. It lacks magnetic sensors and isn’t an over-the-wire system. The lack of magnetic sensors prevents it from using standard magnetic mapping. Instead, electrical impedance mapping was used, which positions the catheter inaccurately; ICE catheter and fluoro imaging had to be used to verify the catheter position.
Because the Catheter 360 is not an Over-the-Wire system, its application is limited to a regional ablation according to Dr. Reddy.
Later in the presentation, starting at 12:30, Dr. Reddy was asked about PLSE’s nano-second PFA technology by someone named “Ed”. The following is their discourse:
Ed: Just a quick question. If you can comment, since we have a lot of data with micro-second pulse field ablation, what are the theoretical benefits to nano-second? Is there less skeletal muscle stimulation or what’s the potential advantage?
Dr. Reddy: Yeah, theoretically there’s less skeletal muscle stimulation, although in these cases we did with general anaesthesia so I have no idea in the patients what it’s gonna be.
In terms of the potential benefit of nano-second, I think we need to learn more, Ed, about this. Some of the theoretical benefits are because it’s nano-second, even though the number of volts is quite high, instead of 2000 volts, this is more like 7-10 thousand volts, but because the duration is so short, the actual amount of joules of energy that enters the tissue is much less than micro-second pulses. So why does that matter? Well, theoretically it helps with catheter construction in terms of the ability to make the type of catheters, but also there’s less thermo-deposition in the tissue, and what that does is it allows you a little more flexibility in terms of how you deliver the energy. You don’t necessarily have to wait as long, for thermal dissipation, and so there’s some potential theoretical benefits. Will they actually translate to actual benefits? I think time will tell. And then the last quick point is, we’ve been talking about the atrium, for which I think micro-second, nano-second both would be OK. But when we get into the ventrical, there are reasons to think that the nano-second would be able to make deeper lesions. So, again this still needs to be proven.
Ed: Any data on the hemolysis effects between the two?
Reddy: I mean, there’s no doubt there’s hemolysis. Same in the sense that they both cause hemolysis. Now how many lesions here translate to one lesion there? I don’t know. Time will tell.
From analyzing Dr. Reddy’s answer above, his most important statement was: “we’ve been talking about the atrium, for which I think micro-second, nano-second both would be OK.”
We interpret this to mean that with PFA in the atrium, both micro-second and nano-second work, there’s no big advantage to one over the other. And the vast majority of PFA procedures are done in the atrium to treat atrial fibrillation.
Dr. Reddy then suggests that nano-second PFA could be used for uncommon, niche, procedures. He stated: “But when we get into the ventrical, there are reasons to think that the nano-second would be able to make deeper lesions. So, again this still needs to be proven.”
PFA has been used in ventricle ablation, but it isn’t common. From a Google search on this topic:
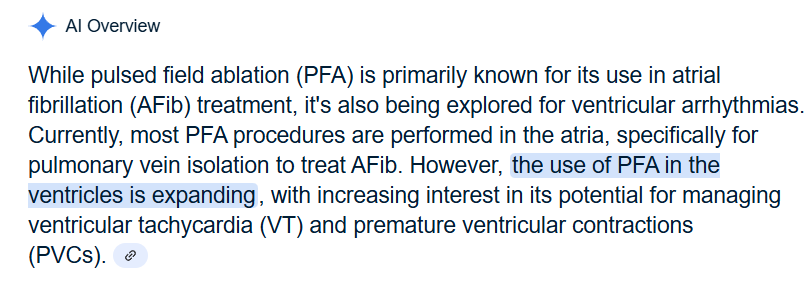
Source: Google
Dr. Reddy claimed “time will tell” if nano-second PFA has any advantages. This presentation was over a year ago. We’ve looked at Dr. Reddy’s public statements since then and we haven’t seen him change his tune on nano-second PFA. PLSE claims that there are advantages to nano-second PFA over micro-second. How many more years does PLSE need to prove whether there’s an advantage or not? The company burns through $50M+ per year.
Farapulse Has Already Studied Nano-Pulse Technology for Pulsed Field Ablation Years Before Pulse Biosciences Did
Farapulse is the market leader in PFA and was acquired by Boston Scientific (BSX) in 2021 for about $500M. It had already been studying nano-second PFA for years before PLSE was ever involved in PFA and before PLSE had any patents for it.
One significant Farapulse patent was filed in 2019. The patent description repeatedly mentions their experiments with both micro-second and nano-second PFA. They even studied sub nano-second times, which is even shorter. The following are some quotes from the patent description:
“In some embodiments, the pulse time duration of each biphasic pulse is in the range from about 0.5 nanosecond to about 20 microseconds.”
“The pulse width/pulse time duration can be in the range from nanoseconds or even sub-nanoseconds to tens of microseconds”
“In some embodiments, the pulse time duration of each biphasic pulse is in the range from about 0.5 nanosecond to about 20 microseconds.”
It’s clear that Farapulse had done thorough diligence and experimentation, and decided that micro-second PFA is better than nano-second PFA. Otherwise, there is nothing stopping them from going the nano-second route.
For someone to be bullish on PLSE and their nano-second PFA, they would have to believe that Farapulse made a mistake in abandoning it. As well as all the other PFA competitors, like Medtronic, who don’t use nano-second PFA.
A Look At Pulse Biosciences Tough Competition in the Pulsed Field Ablation Space
- Both JNJ and Abbott, potential candidates for acquiring PLSE’s PFA technology, have plenty of their own PFA catheters in more advanced stages of development than PLSE.
- JNJ/Biosense Webster – their PFA platform, involved in the inspIRE clinical trial, which is progressing toward US market entry, clinical results has shown promising efficacy and safety, comparable to Medtronic’s PULSED AF study.
- Abbott is developing the Volt PFA system, with early clinical studies underway. CE Mark sub-Analysis suggest good safety and efficacy with a fewer number of PFA applications vs competitors (Faraway, PulseSelct and Varipulse). Its catheter is deflectable and available in over the wire configuration with magnetic distal and proximal sensors. An 8-spline balloon in basket design with impedance-based contact visualization through AutoMark and eField integration for precise lesion tracking. Claims reduced hemolysis. The US VOLT-AF IDE Clinical trials began enrolling patients in April 2024 with a commercial launch is projected around January 2026.
- Kardium
- is closer to product launch and seemingly has lots of promise, including an integrated HD mapping capability. 1-Year PULSE-EU trial positive outcomes were reported a year ago. Kardium’s very long job search page reflects their ambition to do manufacturing and direct sales of the product very soon.
- Adagio Medical
- develops Pulsed Field Cryoablation, the first patient in their PARALELL study was done in 2022; Positive clinicial outcomes just published.
With growing competition strength and the lackluster progress with its own Electrophysiology catheter program, PLSE has to find another thing to keep investors engaged. And it is benign thyroid ablation today!
A Look At The Benign Thyroid Ablation Field
Thyroid ablation has been done using multiple ablation modalities. Overall, ultrasound-guided ablation procedures offer some advantages compared with traditional surgery, such as the elimination of the need for general anesthesia, surgical incision and removal of the thyroid gland. Thermal ablations, such as RF Ablation and Laser Ablation, are currently the mainstream technologies among non-surgical procedures. Microwave and high-intensity focused ultrasound (HIFU) ablation have been gaining traction in recent years, but they are still far from being as widely used as RF ablations. Non-thermal ablation includes Cryo, chemical ablation and Irreversible Electroporation (IRE). These are much less popular than thermal ablations.
Overall, ablation is not as good as surgery in achieving and maintaining euthyroidism, or normal thyroid function, for benign nodules. Thyroid nodules may harbor malignancies, so a biopsy is indicated prior to ablative treatments. Because ablation destroys tissue and thus impedes secondary histological evaluation, ablation currently is not recommended as a first-line treatment for indeterminate nodules. Ablation, therefore, may be used as a viable alternative in some niche applications only, such as small indolent papillary thyroid microcarcinoma (PTMC), recurrent cancers for patients who are unfit for surgery or benign tumors where surgery is contraindicated and there is no risk of cancer presence in the gland.
RF ablation is a dominant technology for thyroid ablation. Tissue necrosis caused by thermal heating is visualized in real time with ultrasound. Care is taken to avoid damage of the laryngeal nerve. Multiple clinical studies indicate successful RF ablation of small glands (<10ml) with a relatively low complication rate for benign nonfunctioning thyroid nodules, papillary thyroid microcarcinoma and recurrent thyroid cancer.
Laser ablation is also popular for similar applications, but data is less robust. MW and HIFU ablation are studied even less. As for IRE, while it is theoretically safer (vs non-thermal treatments) for nearby sensitive structures such as esophagus or nerves, the biggest issue of IRE, that significantly limits its application to thyroids, is that IRE non-thermal ablation is not visible by ultrasounds and other methods, such as computer tomography fluoroscopy, has to be used for IRE probe guidance
Another recent review of clinical tumor ablation in Asia, provides the trend of tumor ablation for different technologies with RF ablation being most popular with more than 50% of all clinical studies published and IRE ablation being least popular with only 1% of all clinical studies published.
IRE (Irreversible Electroporation) technology is the same technology as ms-PFA used in EP cardiac catheter ablation with the only difference it is not a catheter, but a handheld probe. IRE has a history of application in cancers and it has not been very successful. Multiple clinical trials have been performed so far in Prostate, Pancreas, Liver, Kidney and Lung cancers, but IRE has not become a gold standard treatment option in any of these cancers.
One of the most popular devices for IRE ablation of cancers/tumors is Nanoknife, which was acquired by AngioDynamics (ANGO) in 2008. The company invested years in clinical studies using Nanoknife in various applications, such as Liver and Kidney Cancers and is still doing studies in Prostate and Pancreas cancers. Despite 20 years of Nanoknife clinical research and applications, the revenue from Nanoknife is still small and was only about $50M in 2024. This relatively small revenue comes after decades of clinical studies and is from multiple applications. The total market cap of ANGO is only $387M (+$5M in debt) on total revenue of $300M in 2024. Our conclusion is the market is not excited by the future of IRE technology in ablative soft tissue applications.
(Note: AngioDynamics does not report direct sales from Nanoknife. We traced the estimation by analyzing Q1 reports from 2021 to 2025. In 2021, Nanoknife was included with other ablation technologies in Oncology line and its total 9 months sales were $40.3M (Page 29). Assuming the best-case scenario that all oncology sales were due to Nanoknife, its 9-month revenue was $40M in 2021. Starting from 2021, Nanoknife revenue was reported in Medtech group. Increases in Nanoknife 9 month revenue were reported to be 0.8M in Q12022 (Page 26), 1.9M in Q12023 (Page 27) , 3.5M in Q12024 (Page 28) and 0.3M in Q12025 (Page 27). So the maximum total Nanoknife 9 months revenue should be 40+0.8+1.9M+3.5+0.3= $46.5 or $62M on an annual basis.)
Pulse’s Early Clinical Results For Thryroid Ablation Are Weak
Now what about the future of ns-PFA for thyroid ablation? On 3/27/25, from the last PLSE earnings call, the CEO stated:
“We are very pleased by the quality of the preliminary data from our First-In-Human Feasibility Study conducted in Italy and presented at the American Thyroid Association 2024 Annual Meeting. The data presented on 30 patients in three distinct cohorts demonstrated our system’s effectiveness in reducing nodule size.
In Cohort 3, three patients received complete nodule treatment and achieved on average 83% volume reduction at one year and significant reductions in symptoms just one month after treatment without evidence of residual fibrosis or scarring that would routinely accompany radiofrequency ablation.”
It looks like PLSE’s CEO is trying to promote very mediocre data on thyroids. Indeed, the CEO talks about a selected 3 patients from the group of 30 included in the study. And these selected 3 patients operated by the best (and biased) surgical hands had only an 83% reduction after a year.
To call this clinical outcome impressive, to our mind, is laughable. Comparatively, recently published clinical report on Benign Thyroid using RF ablation has a volume reduction of 95.7% at 5 years and of 98.8% in 10 years after a single-session ablation. This set of published data might be on the more optimistic side for RF ablation, but so is the PLSE reported data. It is naïve to think that PLSE has any clinical evidence right now that their technology is better than RF ablation. They need at least 5 years of follow-up and multiple clinical studies to be on par with RF.
The Benign Thryroid Ablation Market Is Small
It seems that the total number of thyroid surgeries in the US, quoted in this 2022 paper, is approximately 140,000 per year. Out of this total number, two-thirds are likely done for benign disease, or about 100,000 surgical procedures per year. It is difficult to know the number of thermal ablations done in the US for benign thyroids, because CMS CPT codes 60660 and 60661 for RF ablation was only recently established in January 2025. Medtronic is a major player providing RF ablation technologies for soft tissue ablation. It is interesting that Medtronic does not even mention RF ablation as an option in its info section for thyroids. It is logical, therefore, to assume that only a small part, perhaps 10-20% of benign invasive treatments, are done today with RF ablation, or around 10K-20K procedures per year in the US. With the RF probe priced at $1,000 USD, the total market is, therefore, around $10-20M only. Confirming our low estimations for the existing thyroid ablation market, PLSE in its investor’s presentation (Slide 14) promotes much needed expansion into “an Untapped Market in Thyroid”.
But what is all this PLSE enthusiasm based on? We do not see much reason for optimism because:
- PLSE prior 2021 failure in the creation of an Untapped Market in Dermatology
- PLSE’s lack of reimbursement code in Thyroids vs existing CPT code for RF ablation
- PLSE’s initial 3 patients’ data on thyroid volume reduction of 83% after one year is not better than that for RF ablation
It seems that PLSE is back to where they were in 2020. At that time they had a similarly promoted dermatology application naively trying to break into an existing market. When the absurdness of their story became obvious in early 2021, the stock went from $45 to below $1 in just one year.
Pulse Has Lost 3 CEOs Over the Past 3 Years, And Hasn’t Explained The Reasons Why
On 9/20/22, PLSE announced Kevin Danahy was appointed as new CEO. The former CEO, Darrin Uecker, got demoted to Chief Technology Officer.
On 5/14/24, PLSE announced Burke T. Barrett has been appointed CEO. The former CEO, Kevin Danahy, got demoted to Chief Commercial Officer.
On 12/6/24 PLSE announced the resignation of its CEO, Burke T. Barrett.
On 1/10/25, PLSE announced the appointment of Paul A. LaViolette as CEO. He was previously the Co-Chairman of the board.
On 2/3/25, PLSE announced the appointment of a new CFO, Jon Skinner.
PLSE doesn’t explain this weird rotating door for CEOs. But we can logically speculate what is going on.
First, Uecker made horrible decisions with respect to the commercialization and FDA approval of NPS. So they brought in Danahy to be the new CEO supposedly specializing in commercialization.
Danahy didn’t understand how to deal with the FDA in cardiac applications when the company made a U-turn towards PFA. He thought they could get their nsPFA clamp approved without clinical studies. On 1/2/24, PLSE announced they filed a 510(K) submission for their clamp. Later that year, the FDA came back with a request for a clinical study for the clamp. Danahy’s misjudgment caused PLSE to waste time when they could’ve started the study right away to get the clamp closer to approval.
Since Danahy failed, they brought in Barrett as the CEO. Barrett has a lot more experience in the cardiology field than Danahy. On the day of his appointment, PLSE closed at $7.69. On the day of his resignation, it closed at $19.75. We believe Barrett likely saw the uphill battle it would be to be the CEO of this company, and the futility of it. He probably would rather just sell his stock that had more than doubled in value and move on to a more fruitful endeavor. Even though he would’ve gotten a nice salary and more stock options, we speculate he decided he didn’t want to spend the next 5 years or so continuing to be dishonest and give false hope to shareholders.
Finally, they appointed LaViolette, a retired corporate executive, as the latest CEO. Before his appointment as CEO, he was already the Co-Chairman of the PLSE board, so he already was familiar with PLSE’s culture of BSing shareholders. He’s here to stay. PLSE’s board probably realized this was an easier route than trying to find a suitable replacement that could also choose to walk away rather than remain the captain of a sinking ship.
Conclusion
PLSE’s NPS technology has a long history of commercial failures which contradict the company’s sky-high valuation of $1B+. As the signs of project delays, un-impressive clinical outcomes and maturing competition become evident in cardiac ablation, PLSE switched investors’ attention to the new application in benign thyroids. This, however, looks to be a repeat of their foray into dermatology, which quickly ended in failure. Similarly, thyroids are currently well served with surgery and RF ablation. The closest analog of PLSE’s NPS technology, IRE technology, failed to achieve any meaningful penetration into this market despite years of clinical research. Given PLSE’s weak initial clinical data in thyroids, we predict a forthcoming commercial failure, inevitably leading to another PLSE stock crash like what happened in 2021 when its dermatology application failed.